Sterile Pyuria – A Vital Indicator of Urinary Tract Infection
STERILE PYURIA
Sterile pyuria is the presence of elevated numbers of white cells (>10/cubic mm) in a urine which appears sterile using standard culture techniques. Often found in female patients with symptoms of urinary tract infection and presence of pyuria but no bacterial growth. However, these results may be misleading for various reasons:
- Standard laboratory culture conditions may not be optimal for growth of atypical
- Laboratory may not report significant growth either because it was not a single organism or recognized urinary
- Less than 100,000 colony-forming units per ml reported, g. may be urine was diluted by high fluid intake or organism may be slow growing. Studies have shown that approximately half of women presenting with symptoms and counts of 100 -10,000 CFU/ml have genuine bladder infections. Presence of pyuria increases significance of a low bacterial count. Cell count per high power field is inaccurate and use of counting chamber or similar gives more accurate results with 10 white cells/mm3 being diagnostic of infection.
Causes of Sterile Pyuria
- Arecently (within last 2 weeks) treated UTI or inadequately treated
- UTI with ‘fastidious’
- Renal tract tuberculosis; Chlamydial
- False negative culture due to contamination with
- Contamination of sample with vaginal
- Interstitial nephritis: analgesic nephropathy, sarcoidosis (lymphocytes not neutrophils).
- Urinary tract
- Renal papillary necrosis: diabetes, sickle-cell disease, analgesic
● Urinary tract ● Polycystic kidneys.
● Interstitial cystitis . ● Prostatitis.
● Corticosteroid ● Balanitis
● Viral infections ● Foreign bodies
● Exercise ( some studies) ● Cyclophosphamide (Cytoxan)
● Recent sexual intercourse in young women ● Use of spermicide in young women
● Urinary catheterization or other instrumentation ● Male patients with AIDS.
● Diabetic women- more likely to have pyuria in some
Other associations include appendicitis, systemic lupus erythematosus and Kawasaki disease.
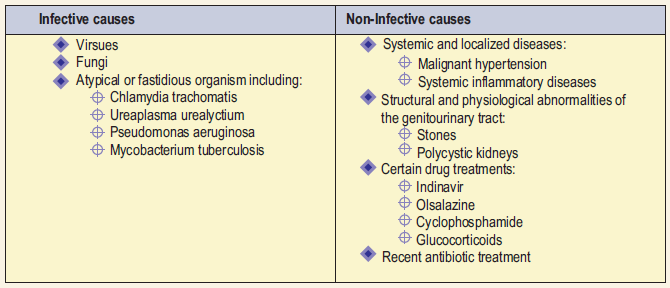
They can be conveniently categorized as:
Epidemiology: Common. Often found in female patients with symptoms of UTI. Also frequent in elderly.
Presentation: Common presentations are:
- UTI: severe dysuria, frequency, urgency, urge incontinence, hematuria, constant suprapubic discomfort, non-specific
- Interstitial cystitis: similar symptoms to UTI with sterile Cystoscopy shows inflammation, sometimes with ulceration. May progress to cause contracture of the bladder. Cause is unknown.
Investigations
- Ask laboratory to culture under conditions allowing identification of fastidious or slow growing
- Always consider TB: culture for AFB’s (3 early morning urines).
- With urine obtained direct from the bladder, any organism grown is significant and should be treated with a prolonged course of appropriate
- Otherwise cystoscopy to exclude non-infective
Before further investigation, it is important to ensure that repeat specimens are collected appropriately. A mid-stream clean catch sample can help avoid contamination with WBCs from vaginal or prostatic secretions. Culture-negative results can be seen in a single sample if the patient has taken antibiotics immediately before giving the sample. But if persistent sterile pyuria is seen and the patient has clinical symptoms consistent with UTI, a further specimen should be taken and the culture repeated to check for fastidious, atypical or resistant organisms. Standard laboratory media kill many of the possible pathogens so the laboratory must be informed of the clinical suspicion of atypical or fastidious organisms.
Sterile Pyuria and SLE
The results of various studies suggest that isolated hematuria and isolated pyuria are associated with active renal and non-renal disease activity. Thus they should be considered manifestations of active SLE.
Sterile Pturia and Tuberculosis
In the past “sterile” pyuria suggested the existence of tuberculosis of the urinary tract. In common with all forms of the disease, the incidence of genitourinary tuberculosis has declined but “Sterile” pyuria is still common. Various studies have been carried out in the past to establish the relationship between the two. The incidence of urinary tract tuberculosis in patients whose urine showed “sterile” pyuria is low, and so the cost effectiveness of surveying all such samples must be equally low. The practice of the laboratory therefore may not be to examine every specimen showing “sterile” pyuria for Mycobacterium tuberculosis but to advise local practitioners to consider the diagnosis of urinary tract tuberculosis when persistent unexplained “sterile” pyuria is observed. When to investigate for tuberculosis? The association of pyuria and microhematuria associated with acid urine, without identification of a putative organism with routine microbiologic studies, should prompt evaluation for tuberculosis.
Management
The finding of pyuria without bacteriuria can be a diagnostic challenge and warrants further investigation. A careful history and physical examination can help determine the cause of sterile pyuria. Always consider TB or non-infective cause and don’t prescribe antibiotics if infection is not proven or otherwise suspected.