Hypothyroidism – Etymology, Causes and Test Results
INTRODUCTION
Hypothyroidism is defined as a deficiency in thyroid hormone secretion and action that produces a variety of clinical signs and symptoms of Hypometabolism.
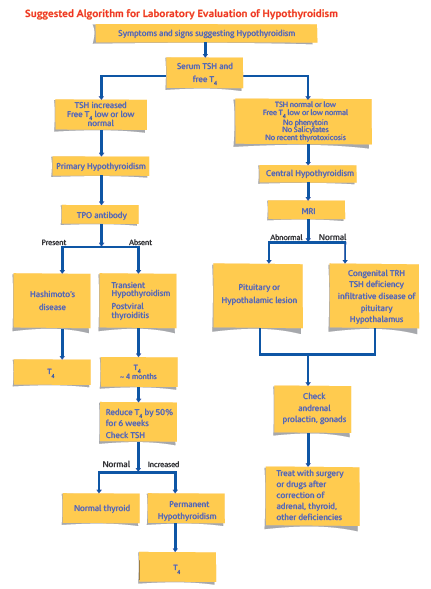
- Overt Hypothyroidism is defined as an elevated serum TSH concentration (usually above 10 mIU/L) and reduced free Thyroxine concentration (fT4)
- Subclinical Hypothyroidism is defined as serum TSH above the upper reference limit in combination with a normal free Thyroxine (fT4)
Prevalence
According to a projection from various studies on Thyroid disease, it has been estimated that about 42 million people in India suffer from Thyroid diseases. The prevalence of Hypothyroidism was 3.9%. The prevalence of subclinical Hypothyroidism was 9.4%. In women, the prevalence was higher, at 11.4%, when compared with men, in whom the prevalence was 6.2%. The prevalence of subclinical Hypothyroidism increased with age. About 53% of subjects with subclinical hypothyroidism were positive for anti-TPO antibodies.
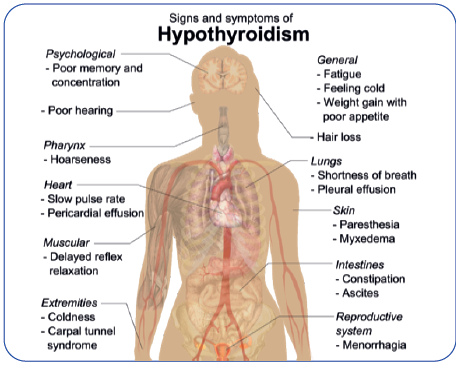
CLINICAL PRESENTATION
Hypothyroidism can affect all organ systems & these manifestations are largely independent of the underlying disorder but are a function of the degree of hormone deficiency.
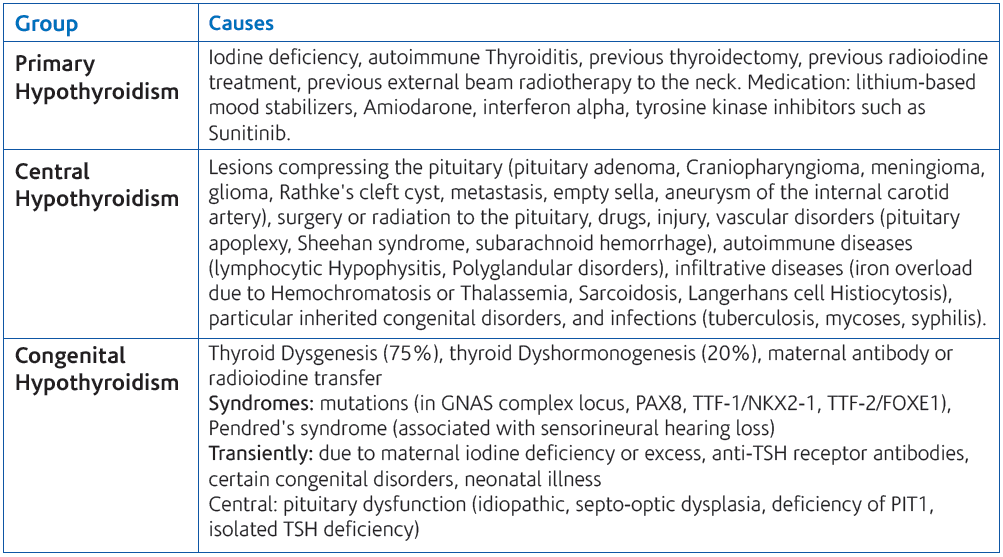
CAUSES OF HYPOTHYROIDISM
HASHIMOTO’S THYROIDITIS
Hashimoto’s Thyroiditis is an autoimmune disease in which the thyroid gland is attacked by a variety of cell and antibody-mediated immune processes, causing primary Hypothyroidism. The resulting inflammation from Hashimoto’s disease, also known as Chronic Lymphocytic Thyroiditis, often leads to an underactive Thyroid gland (Hypothyroidism).
The diagnosis of Hashimoto’s Thyroiditis is supported by recognition of autoantibodies against TPO or Thyroglobulin. 90% of patients with Hashimoto’s Thyroiditis have anti-TPO antibodies and anti-Thyroglobulin antibodies, making these antibodies excellent markers for Hashimoto’s Thyroiditis. Anti-TPO antibody positivity is more common at the time of diagnosis than anti-Thyroglobulin antibody.
Hypothyroidism in pregnancy
Convincing data suggest that pregnant women who are positive for Thyroid autoantibodies (especially anti-TPO antibodies) leads to higher frequency of miscarriage (13.8%) than is seen in pregnant women who lack anti-TPO antibodies (2.4%), and that T4 treatment of the anti-TPO antibody positive group reduces the risk of miscarriage to approximately 3.5%.
Over Hypothyroidism (OH) in pregnancy is defined as an elevated TSH (>2.5 mIU/L) in conjunction with a decreased FT4 concentration. Women with TSH levels of 10.0 mIU/L or above, irrespective of their FT4 levels, are also considered to have OH.
Sub-clinical Hypothyroidism (SCH) in pregnancy is defined as a serum TSH between 2.5 and 10 mIU/L with a normal FT4 concentration.
Isolated Hypothyroxinemia (IH) is defined as a normal maternal TSH concentration in conjunction with FT4 concentrations in the lower 5th or 10th percentile of the reference range.
Prevalence
- 10%-20% of all pregnant women in the first trimester of pregnancy are Thyroid Peroxidase (TPO) or Thyroglobulin (Tg) antibody positive and Euthyroid
- 16% of the women who are Euthyroid and positive for TPO or Tg antibody in the first trimester will develop a TSH that exceeds 4.0 mIU/L by the third trimester, and 33%-50% of women who are positive for TPO or Tg antibody in the first trimester will develop postpartum Thyroiditis
- 2%–3% of apparently healthy, non-pregnant women of childbearing age have an elevated serum TSH. Among these healthy non-pregnant women of childbearing age it is estimated that 0.3%-0.5% of them would, after having Thyroid function tests, be classified as having OH, while 2%–2.5% of them would be classified as having SCH
Specific adverse outcomes associated with maternal Hypothyroidism include:
- An increased risk of premature birth, low birth weight, and miscarriage. Such patients carry an estimated 60% risk of fetal loss when OH was not adequately detected and treated
- Negro and colleagues published data suggesting SCH also increases the risk of pregnancy complications in anti-thyroid peroxidase antibody positive (TPOAb+) women
- Negro et al. reported a significantly higher miscarriage rate in TPOAb+_ women with TSH levels between 2.5 and 5.0 mIU/ L compared with those with TSH levels below 2.5 mIU/L
Recommendations:
- Women who are positive for TPOAb and have SCH should be treated with LT4
- Women with SCH in pregnancy, who are not initially treated, should be monitored for progression to OH with a serum TSH and FT4 approximately every 4 weeks until 16-20 weeks gestation and at least once between 26 and 32 weeks gestation
- Isolated Hypothyroxinemia should not be treated in pregnancy
Recommendations
- Anti-Thyroid Peroxidase Antibody (TPOAb) measurements should be considered when evaluating patients with subclinical Hypothyroidism.
- If anti-thyroid antibodies are positive, Hypothyroidism occurs at a rate of 4.3% per year versus 2.6% per year when anti-thyroid antibodies are negative.
- Assessment of serum free T4, in addition to TSH, should be considered when monitoring L-thyroxine therapy.
- Treatment based on individual factors for patients with TSH levels between the upper limit of a given laboratory’s reference range and 10 mIU/L should be considered particularly if patients have symptoms suggestive of Hypothyroidism, positive TPOAb or evidence of atherosclerotic cardiovascular disease, heart failure, or associated risk factors for these diseases.
- Patients whose serum TSH levels exceed 10 mIU/L are at increased risk for heart failure and cardiovascular mortality, and should be considered for treatment with L-thyroxine.
- Euthyroid women (not receiving LT4) who are TPOAb + require monitoring for Hypothyroidism during pregnancy. In addition to the risk of Hypothyroidism, it has been described that being TAb + constitutes a risk factor for miscarriage, premature delivery, Perinatal death , post-partum dysfunction, and low motor and intellectual development (IQ) in the offspring.
TEST RANGE AVAILABLE
References:
- Indian Journal of Endocrinology & Metabolism. 2011 Jul; 15(Suppl2): S78–S81.
- Williams text book of Endocrinology, Eleventh edition
- Tietz Textbook of Clinical Biochemistry, Fifth Edition
- Clinical Practice Guidelines for Hypothyroidism in Adults: Cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association
- Negro R, Schwartz A, Gismondi R, Tinelli A, Mangieri T, Stagnaro-Green A 2010 Universal screening versus case finding for detection and treatment of thyroid hormonal dysfunction during pregnancy. J Clin Endocrinol Metab 95:1699–1707.
- Negro R, Schwartz A, Gismondi R, Tinelli A, Mangieri T, Stagnaro-Green A 2010 Increased pregnancy loss rate in thyroid antibody negative women with TSH levels between 2.5 and 5.0 in the first trimester of pregnancy. J Clin Endocrinol Metab 95:E44–8
 National Customer Care : Tel: 011-3988-5050
National Customer Care : Tel: 011-3988-5050
Corporate Office: 12th Floor, Tower B, SAS Tower, Medicity,
Sec- 38, Gurgaon- 122 001, Haryana
Tel: 0124- 3016 500 | Fax: 0124- 42344668
National Reference Lab: Sector-18, Block-E, Rohini, New Delhi- 110 085
www.lalpathlabs.com
doctorfeedback@lalpathlabs.com
Please follow up at : http://www.twitter.com/lalpathlabs : http://www.facebook.com/lalpathlabs