Autoimmune Arthritis: Symptoms, Types & Diagnosis
What is autoimmune arthritis?
Autoimmune arthritis refers to the types of arthritis in which a person’s immune system attacks their body. It causes inflammation, pain, and stiffness in a joint.
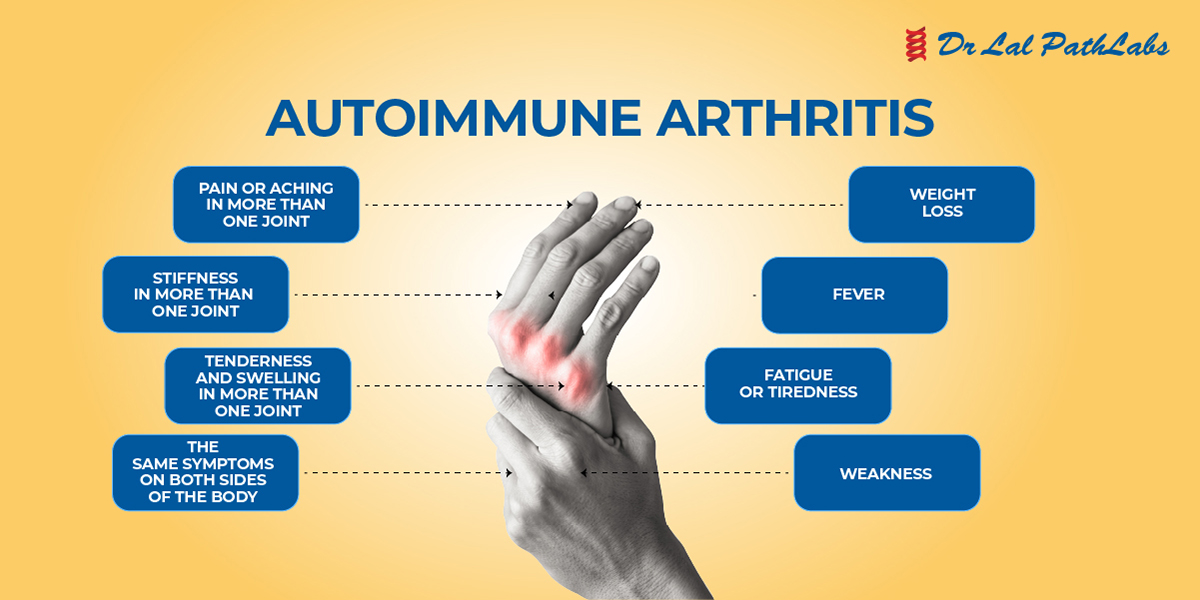
What are the symptoms of autoimmune arthritis?
Some common symptoms of autoimmune arthritis are:
- Fever
- Joint pain
- Stiffness
- Swelling
- Weakness
- Dry mouth
- Weight loss
- Anemia
- Dry eyes, itchy eyes
What are the risk factors for autoimmune arthritis?
There are several risk factors that can increase the likelihood of developing autoimmune arthritis.
- Gender: Women are at greater risk of developing rheumatoid arthritis than men.
- Age: Autoimmune arthritis can develop at any age, but people mostly notice the symptoms between the ages of 49 and 60.
- Family history: If someone in your family has autoimmune arthritis, then there are more chances that you may also have it.
- Smoking: Smoking can increase your chances of having autoimmune arthritis.
What are the types of autoimmune arthritis?
Some of the common forms of autoimmune arthritis are:
- Rheumatoid Arthritis: RA usually causes swelling and pain in the hands, feet, and wrists.
- Spondylarthritis: This type of arthritis affects the spine and joints. Some common types include reactive arthritis, axial spondylarthritis, and enteropathic arthritis.
- Juvenile arthritis: It can cause joint pain, eye inflammation, fever, and rashes.
- Palindromic rheumatism: It causes inflammation around the joints and often affects the areas around the fingers, wrists, and knees. It causes symptoms such as pain, swelling, and fever.
How is autoimmune arthritis diagnosed?
A physician who diagnoses arthritis is called a rheumatologist. The rheumatologist will diagnose arthritis based on several factors, such as medical history, symptoms, etc. The doctor will recommend the following blood tests to look for inflammation and blood proteins that are linked to arthritis.
- Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) tests: to confirm inflammation in the joints.
- Rheumatoid factor (RF): This is an antibody found in most people affected with arthritis.
- Imaging tests: X-ray, ultrasound, or MRI can confirm bone erosion.
How is autoimmune arthritis treated?
Autoimmune arthritis can be treated symptomatically. The doctor will recommend treatment based on the person’s symptoms, type of arthritis, and overall health.
Medications
The mild form of autoimmune arthritis can be managed by taking nonsteroidal anti-inflammatory drugs. For some forms of arthritis, the doctor may recommend medicines called disease-modifying antirheumatic drugs (DMARDs).
Lifestyle changes
The doctor will also recommend lifestyle changes that can benefit a person with an autoimmune disorder.
- Getting regular exercise: Walking, water aerobics, and other low-impact aerobic exercise are beneficial for arthritis.
- Quitting smoking: Cigarette smoking can worsen the symptoms of autoimmune arthritis.
- Eating a well-balanced diet: A nutritious diet can help maintain a moderate weight, putting less pressure on painful joints.
- Regular sleep: Not getting regular sleep may worsen flares and other symptoms.
Self Care
You play an important role in controlling your autoimmune arthritis. Follow these self-care tips to help keep your symptoms in check.
Quit Smoking
Smoking can worsen your arthritis symptoms, and it also makes it difficult to stay active. It can also increase the risk of other health problems, especially heart disease.
Manage weight
Losing weight can be difficult, but fat cells release proteins that cause inflammation. It makes the joint pain worse, and your medicine may not work properly. Even a little weight loss can make a difference.
Physical Activity
Exercise helps in reducing inflammation, and strengthening your bones, is good for your heart and lungs, relieves pain, improves your mood and sleep, helps with weight loss, and keeps joints moving. Aim for 30 minutes of cardio and get help from a physical therapist if you have not exercised for a long time.
Good Sleep
Pain in joints makes it hard to fall asleep, and a lack of sleep makes you more sensitive to pain. Most sleep problems in people with RA are related to anxiety and uncontrolled RA symptoms:
- Take your medicines on time.
- Avoid caffeine late in the day.
- Limit screen time before bed
- Exercise during the day
Manage stress
Stress may trigger RA flares. You can manage stress by:
- Meditating
- Practising yoga
- Taking walks in nature
- Spend time with your pets
- Listening to music
Frequently Asked Questions
1. What type of arthritis is autoimmune?
There are four types of autoimmune arthritis:
- Rheumatoid Arthritis: RA usually causes swelling and pain in the hands, feet, and wrists.
- Spondylarthritis: This type of arthritis affects the spine and joints.
- Juvenile arthritis: It can cause joint pain, eye inflammation, fever, and rashes.
- Palindromic rheumatism: It causes inflammation around the joints and often affects the areas around the fingers, wrists, and knees
2. What is the most common form of autoimmune arthritis?
Rheumatoid arthritis is the most common type of arthritis. Its symptoms include joint pain, stiffness, swelling, and decreased flexibility of the joints.
3. What is the cause of autoimmune arthritis?
The exact cause of autoimmune arthritis is not known, but the immune system starts attacking its own healthy tissues in the joint, which causes inflammation, swelling, and other symptoms.
4. Can autoimmune arthritis be cured?
Although there is no cure for autoimmune arthritis, its symptoms can be managed by medications and by making certain lifestyle changes.
5. How is autoimmune arthritis diagnosed?
The rheumatologist will diagnose arthritis based on several factors, such as medical history, symptoms, etc. The doctor will recommend the ESR test, C-reactive protein test, and Rheumatoid factor (RF) test to look for inflammation and blood proteins that are linked to arthritis.
Disclaimer:
This blog is for informational purposes only and should not be construed as advice or as a substitute for consulting a physician. It is not a substitute for medical advice or treatment from a healthcare professional.