All About Newborn Screening
What is Newborn Screening?
Newborn screening is a set of blood tests to look for evidence of certain endocrine and genetic disorders. Newborn screening has the potential to identify risk of certain diseases before the appearance of clinical symptoms. Early detection and early treatment can prevent mental retardation, spasticity, serious illness, and premature death.
World Statistics
According to World Health Organisation (WHO), 140 million children are born every year, of which 5 million children die in the first month of life in the developing countries and 4 million children are born with some genetic abnormality. Whenever a child dies due to unknown cause, it is termed as Sudden Infant Death Syndrome (SIDS). It is estimated that 25-30% of such children are unable to thrive due to metabolic disorders. In other words, 25-30% of SIDS are a result of treatable metabolic disorders. These children suffer from life threatening complications occurring as a result of disturbance in the metabolic pathway. The diagnosis can be preempted & the complications well controlled by newborn screening.
A study by March of Dimes has revealed that in 2007, almost 90 percent of newborns (about 4 million babies) in the United States were tested for almost 29 genetic disorders.
Indian Statistics
People of India constitute more than one-sixth of the World’s population, but statistically they have been under-represented in newborn screening. About 4 percent of the population in India suffers from mental retardation and 5-15% of the sick newborns have a metabolic problem. It is estimated that 1 in 2000 Indian newborns suffer at birth from some kind of metabolic disorder. The World ratio for the same category is 1 in 3600. An estimated 3,90,000 children with G6PD deficiency and 9760 with aminoacid disorders are born in India each year ( Dr IC Verma, Community Genetics 2002;5:192-196). Dr Radha Rama Devi, in her study (Newborn Screening in India. Indian J Pediatr 2004;71:157-160) observed a high prevalence of inborn errors of metabolism ( metabolic genetic disorders) to the extent of 1 in every thousand births. A prevalence of congenital hypothyroidism 1 in 1700 , congenital adrenal hypothyroidism 1 in 2575 and aminoacid disorders 1 in 3600 was observed. Dr Mamta Muranjan from Mumbai detected 13.85% of confirmed cases of organic disorders in four year study from 1995-1998 (Indian Pediatrics 2001;31:518-524).
Even if we consider a meager 2% of live births in India to develop metabolic genetic disorders, then 500,000 affected children are born every year.
Disorders Included in Newborn Screening Panel
- Biotinidase Deficiency
- Congenital Adrenal Hyperplasia
- Congenital Primary Hypothyroidism
- lG6PD Deficiency
- Cystic Fibrosis
- Galactosemia
- 30Disorders of Aminoacids, Organic acids & Fatty acid oxidation by Tandem Mass Spectrometry
Biotinidase Deficiency:
Biotinidase deficiency is a disorder caused by the lack of enzyme biotinidase. Babies with partial or total deficiency need more biotin than normally found in the diet. Biotin is a water soluble vitamin of the B complex group.
Clinical manifestations: Children with biotinidase deficiency may present with clinical symptoms as early as first week of life, but usually begin to show clinical symptoms between 3 to 6 months of age. If untreated, they develop a variety of cutaneous and neurological abnormalities. Affected children usually have myoclonic seizures,hypotonia, seborrheic or atopic dermatitis, partial or complete alopecia.
Laboratory findings include ketolactic acidosis, organic aciduria, mild hyperammonemia. Metabolic acidosis can result in coma and death.
Treatment if initiated sufficiently early can prevent the occurence of clinical symptoms. Once neurological symptoms appear, it is not possible to reverse the damage with treatment. Sensorium & hearing loss is common with profound biotinidase deficiency and is usually irreversible.
Screening is done by assessment of biotinidase activity on whole blood spotted on filter paper. Cases detected as profound or partially deficient, are confirmed by testing biotinidase activity in serum.
Benefit of Screening: Observation at LPL is that biotinidase deficiency is the most common disorder. Once symptoms have occurred, some of the findings particularly neurologic are not reversible with therapy.
Congenital Adrenal Hyperplasia:
Congenital adrenal hyperplasia (CAH) is a disorder of adrenal cortex. Majority of CAH cases are attributable to 21-hydroxylation defect in the adrenal cortex. This results in low concentration of aldosterone & cortisol and elevated 17-hydroxyprogesterone (17OHP). Screening for CAH measures the level of 17-hydroxyprogesterone (17OHP).
Types
- “Classic severe” salt wasting (SW) form
- “Classic, less severe” simple-virilizing (SV) form
- “Mild” non classic form
Clinical Manifestations
Neonates affected with SW form are at risk of adrenal crisis. Crisis can manifest as poor feeding, vomiting, loose stools or diarrhoea, weak cry, failure to thrive, dehydration and lethargy. These symptoms may not be evident until serum sodium concentrations are below 125mEq/L. Some affected infants may suffer from brain injury or learning disabilities. Female newborns affected with SW forms have ambiguous genitalia. Affected male infants do not exhibit any physical signs at birth. Therefore, without newborn screening & in the absence of a positive family history, all affected males and few females remain undiagnosed until adrenal crisis.
Patients affected with SV form manifest adrenal –insufficiency symptoms when subjected to stress and are diagnosed much later when symptoms of virilization, precocious pseudopuberty or growth acceleration occurs. Late discovery of correct gender can cause distress to the family and patient. Mild 21-OH deficiency produces no symptoms at birth and manifest as premature sexual hair, acne and mild growth accleration in childhood and hirsutism, excessive acne, menstrual disorder and infertility later in life. Mild disorders may be missed by newborn screening.
Benefits of newborn screening are:
- Prevent life threatening adrenal crisis. Adrenal crisis can cause shock, brain damage, and death.
- Prevent male sex assignment in virilized female newborns
- Prevent progressive effects of excess adrenal androgens, which can cause short stature and psychosexual disturbances.
Worldwide newborn screening data has shown that screening prompted early diagnosis of CAH even before clinical suspicion in 67% of newborn infants with CAH.
Congenital Hypothyroidism:
Congenital hypothyroidism is caused due to deficiency of thyroid hormone since birth. CH is one of the most common and treatable causes of mental retardation. Some infants are normal at birth due to protection by maternal thyroid hormone.
Clinical Manifestations
Males and females are affected equally. The severity of symptoms and physical findings correlates with the degree of hypothyroidism. Clinical symptoms in the first week of life are usually not apparent. The affected infants suffer from feeding problems, constipation, lethargy, hoarse cry, prolonged jaundice, cool, dry mottled skin, coarse facies with large open fontanelles, umbilical hernia & delayed development. Mental deficiency can be prevented by newborn screening and prompt treatment with thyroid hormones.
Screening is performed by measuring TSH level. Some infants may have a slight increase in TSH. These patients need to be observed and thyroid function test should be repeated after a few months.
Cystic Fibrosis
Cystic fibrosis is a multisystem disease affecting lungs, pancreas, intestine, liver & sweat glands. Cystic fibrosis was thought to be rare in India. However published reports indicate that cystic fibrosis is probably more common than previously thought but is underdiagnosed or missed in majority of the cases ( Ahuja AS & Kabra SK. Cystic fibrosis: Indian Experience. Indian Pediatrics.2002:39:813-818). According to Christine Noke, Director Cystic Fibrosis Worldwide Programme,40,000 Indians in United States and 28,000 Indians in United Kingdom suffers from Cystic fibrosis and there is possibility of 100,000 patients in India ( www.cfww.org). The total load due to Cystic fibrosis could be more than many European countries (Kapoor V, Shastri SS, Kabra M etal. Carrier frequency of F508del mutation of Cystic fibrosis is noted in Indian population ( Journal of Cystic Fibrosis 2006;5:43-46). Cystic fibrosis patients are mostly treated as tuberculosis and the acute exacerbations labeled as ‘bronchopneumonia” (Dr Meenu Singh, PGI Chandigarh. www.cfww.org).
Clinical Manifestations
Cystic fibrosis usually presents in infancy. In about 10-20% cases, the first symptom of disease appear soon after birth.Symptoms and severity of disease differ from person to person but the basic problem remains the same i.e. the glands which produce or secrete sweat and mucus do not function properly. This results in unusually thick mucus, which clogs lungs. Mucus also affects the pancreas by blocking digestive enzymes, which are needed for breakdown & assimilation of food. Some patients have both respiratory and digestive problems while some have respiratory problems only.Cystic fibrosis does not affect intelligence.
Most common symptoms are:
- Meconium ileus
- Malnutrition
- Poor growth
- Frequent respiratory infections
- Breathing difficulties
- Lung damage
- Nasal polyps
- Pneumothorax (rupture of lung tissue and trapping of air between the lungs and chest wall)
- Rectal prolapse
- Hemoptysis ( coughing of blood)
- Abdominal pain and discomfort
- Liver disease, inflammation of the pancreas
- Infertility
Screening: Detection of Cystic fibrosis in newborns depends on the presence of immunoreactive trypsinogen (IRT). IRT levels tend to remain raised for several months in babies with CF, whereas in false positive cases, values usually return to normal within first few weeks of life ( Wilcken B, Brown ARB, Urwin R, Brown DA. Cystic fibrosis screening by dried blood trypsin assay results in 75,000 infants. J Pediatr 1983;102:383-387). In babies with meconium ileus, the IRT levels may not be elevated. High frequency of heterozygotes have been reported among neonates with elevated IRT and normal sweat chloride level ( CastellanicC, PicciL, ScarpaM, DecheechiMC etal. Cystic fibrosis carriers have higher neonatal immunoreactive trypsinogen values than non-carriers. Am J Med Genet A2005;135(2):142-144).
Benefit of Screening: CF babies are normal with no evidence of lung disease or pancreatic insufficiency. Symptoms develop over first 3-6 months of life. By the time children are diagnosed clinically with CF, they are already seriously ill with lung disease and significant malabsorption problems. Before screening test was introduced, the average age of children without known sibling with CF was about 18 months (Wilcken B,Towns SJ,Mellis CM. Diagnostic delay in cystic fibrosis:lesson from newborn screening. Arch Dis Child 1983;58:863-866). Better treatment methods developed over the past 20 years have increased the life span of CF patients. Early diagnosis helps in improved height and weight due to early initiation of therapy which includes pancreatic enzyme, fat soluble vitamin and salt supplementation ( Farrell PM, Kosorok MR, Rock MJ etal. Early diagnosis of cystic fibrosis through neonatal screening prevents severe malnutrition and improves long term growth. Wisconsin Cystic Fibrosis neonatal screening study group. Pediatrics 2001;107:1-13)
Galactosemia
Galactosemia is a disorder in which galactose cannot be broken down in the body. Galactose is found in breast milk, many formulas and milk products. Under normal conditions, galactose is released by the digestion of lactose and is converted to glucose as well as fructose in the body. In galactosemia, there is genetic defect in conversion of galactose to glucose. Increased concentration of galactose in blood can harm the baby’s eyes, liver and brain causing cataract & mental retardation. Affected infants may die in the neonatal period due to Escherichia coli sepsis or later due to cirrhosis of liver.
Newborn screening tests: Test for galactose depends on the infant’s diet; therefore it is important that the infant is receiving galactose-containing formula or breast milk before testing.
Benefit of Screening: Exclusion of galactose from the diet can prevent cataract, mental retardation and other life threatening complications.
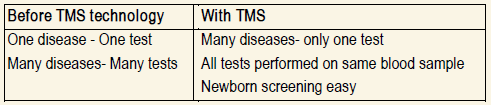
TANDEM MASS SPECTROMETRY
Disorders of Aminoacids, Organic acids & Fatty acid oxidation can be tested by Tandem Mass Spectrometer (TMS).
“That some infants are not being caught and treated when possible is a national tragedy and tandem mass spectrometry should be standard care for all newborns, much as blood pressure test is a part of every medical checkup”- Harry Hannon, Director New Born Screening Services, CDC
Source: The Wall Street Journal, 2004 Why test with Tandem Mass Spectrometer?
- More cases of inborn errors of metabolism are diagnosed by screening with tandem mass spectrometry than are diagnosed clinically. (New England Journal of Medicine 2003; 348: 2304-12).
- lSIDS or Metabolic Disorder?: TMS can differentiate
- 3-6% of SIDS are due to inherited disorders of Fatty Acid Oxidation, (Clinical Chemistry; June 2001:47 (7)1166-1182)
What Analytes are measured by Tandem Mass Spectrometry?
Aminoacids: building blocks of proteins
Carnitine: transportation system for fats in and out of mitochondria l
Acylcarnitine: Acylcarnitines are identified by the size of fat molecule attached to it and categorised simply as short, medium amd long chain. The important medium sized fat attached to carnitine that is measured in MCAD is eight carbon fatty acid known as Octanoylcarnitine and is abbreviated as C8
Disorders detected by TMS
I. Aminoacid Disorders:
- Urea cycle disorders
- Homocystinuria
- Hypermethioninemia
- Non-ketotic hyperglycinemia
- Hyperammonemia, Hyperornithinemia,Homocitrullinuria
- MSUD
- PKU
- Trosinemia
II. Organic Acid Disorders:
- Gutaric acidemia type 1
- Isovaleric acidemia
- 3-ketothiolase deficiency
- 3-MethylcrotonylC0A carboxylase deficiency
- 3-Methylglutaconyl CoA hydratase deficiency
- Mutiple carboxylase deficiency
- Beta-Ketothiolase deficiency
- Methylmalonic acidemia
- Methylmalonic acidemia with homocystinuria
- Propionic acidemia
III. Fatty acid Oxidation Disorders:
- Shortchain acyl CoA dehydrogenase deficiency (SCAD)
- Medium chain acyl CoA dehydrogenase deficiency (MCAD)
- Mitochondrial trifunctional protein deficiency
- Longchain 3-hydroxy acyl CoA dehydrogenase deficiency (LCHAD)
- Very long chain acyl CoA dehydrogenase deficiency ( VLCAD)
- Carnitine transport defect
- Carnitine palmitoyl transferase deficiency type 1 (CPT 1)
- Carnitine palmitoyl transferase deficiency type 2 ( CPT 2)
- Gutaric acidemia type 2
- Carnitine acylcarnitine translocase deficiency
Sensitivity, Specificity, Positive Predictive Value of TMS
- Sensitivity close to 100% with high positive predictive value (PPV)
- Classical MSUD
- UCD
- Tyrosinemia
- PKU
- Earlyonset organic acidemias
- Fatty acid oxidation disorders (Ref:J Inherit Metab Dis (2007)30:129-133)
False Positive Rate (TMS)
lLow
l0.2-0.33 % of babies screened needed further testing (Ref:J Inherit Metab Dis (2007)30:129-133)
What is the Screening sample?
5 drops of blood are taken from the baby’s heel. Baby’s heel is pricked with a lancet and drops of blood are collected on special filter paper.
When should the newborn screening sample be collected?
Infant must be 48 hours of age or older in order to obtain a satisfactory sample for screening. Ideal time is 4 days of age. Sample should be taken prior to administering antibiotics or transfusing blood or blood products.
What is the cutoff age for an infant when accepting sample for newborn screening? Till one month of age except for disorders by TMS. Test methodologies for other tests are set to obtain valid values till 30 days of age. Result values of tests carried out beyond 30 days may overlap considerably making it difficult to distinguish presence or absence of disorders.
Factors which affect Result & Interpretation:
- Size of blood spot
- Bood for test aspirated from iv catheter
- Intravenous fluid hydration with dextrose prior to collection of sample can flush out short lived active acylcarnitine metabolite from the intravascular blood
- stream
- IVfluid
- Bood transfusion
- Low Protein diet
- Supplemented with aminoacids
- Drugs such as valporic acid, MCT Oil, antibiotics containing a derivative of pivalic acid
How long to wait to screen an infant who has been transfused?
Given the presumption that the mean age of RBC’s of the transfused blood is 60-80 days, it is suggested that sample should be collected 60 days after discontinuation of transfusion.
What to do for an infant who needs antibiotics prior to 24 hours of age?
Sample taken from infants receiving antibiotics at the time of collection may yield false results. Sample should be collected prior to starting antibiotic therapy or 24 to 36 hours after discontinuation of antibiotic therapy.